A. Baranova, Thuy Tran, Rohini Mehta, A. Birerdinc. Z. M. Younossi
This is a collaborative project between
School of Systems Biology, College of Science,George Mason University, Fairfax, VA
Translational Reseach Institute, Inova Hospital, VA
This Systematic Review manuscript is published in 2011: "Systematic review: association of polycystic ovary syndrome with metabolic syndrome and non-alcoholic fatty liver disease". Aliment Pharmacol Ther. 2011 Apr;33(7):801-1
Background
Polycystic ovary syndrome (PCOS) is a common disorder for women of child-bearing age and is associated with metabolic syndrome (MS).
Aim
To assess the literature for associations between Polycystic ovary syndrome and
non-alcoholic fatty liver disease (NAFLD).
Methods
We performed a systematic review using PubMed-search for peer-reviewed articles
related to Polycystic ovary syndrome and NAFLD. Articles were summarised and
grouped according to different sections defining interactions of Polycystic ovary
syndrome with metabolic syndrome and non-alcoholic fatty liver disease as well as
risk factors, pathogenic pathways and treatment options.
Results
Obesity is a common factor involved in both Polycystic ovary syndrome and non-alcoholic fatty liver disease. Obesity causes non-alcoholic fatty liver disease and aggravates hirsutism and menstrual disorders in Polycystic ovary syndrome. Insulin
resistance (IR), a hallmark of metabolic syndrome is observed in 50–80% of
women with Polycystic ovary syndrome and patients with non-alcoholic fatty liver
disease. Recent findings suggest that women with Polycystic ovary syndrome
may be at risk for developing non-alcoholic fatty liver disease and conversely, non-alcoholic fatty liver disease may be a risk for Polycystic ovary syndrome. Based on
the association of Polycystic ovary syndrome and other metabolic abnormalities,
such as IR, hyperandrogenism, obesity and non-alcholic fatty liver disease, the candidate genes have been speculated for Polycystic ovary syndrome. Closer scrutiny
of these genes placed most of their proteins at the crossroads of three highly interrelated conditions: metabolic syndrome, obesity and non-alcholic fatty liver disease.
In most studies, the prevalence of both Polycystic ovary syndrome and non-alcoholic fatty liver disease rises proportionally to the degree of IR and increases in the
mass of adipose tissue.
Conclusions
Non-alcoholic fatty liver disease is considered as the hepatic manifestation of metabolic syndrome. Similarly, it seems appropriate to consider Polycystic ovary syndrome as the ovarian manifestation of metabolic syndrome. Both these conditions
can co-exist and may respond to similar therapeutic strategies.
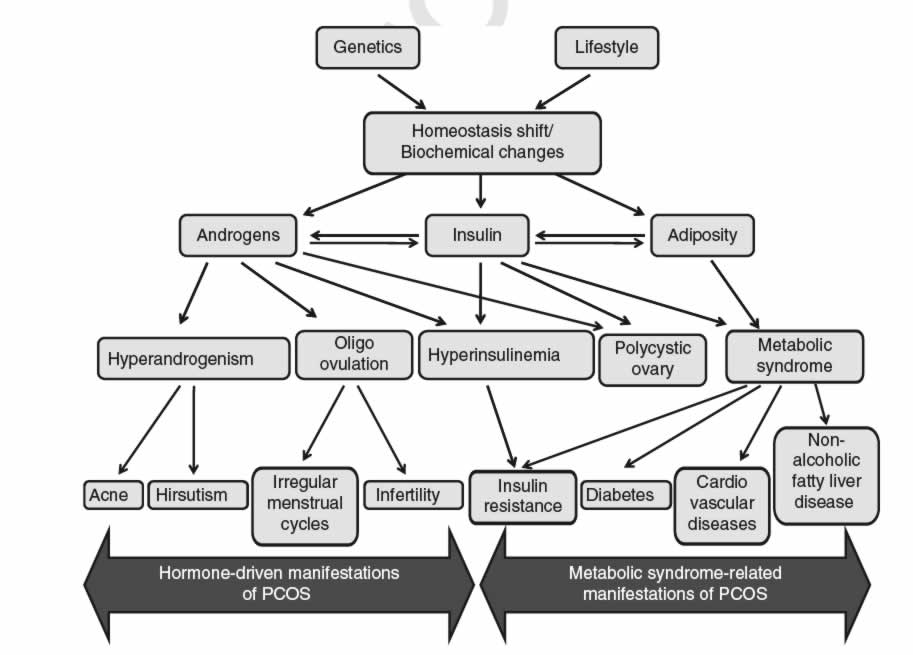
Figure 1. An interplay of various components of PCOS phenotype
A comparison of gene expression profiles for obesity-related genes and inflammatory cytokine in adipose tissue of patients with and without clinical polycystic ovarian syndrome (PCOS) diagnosis.
Thuy Tran, Rohini Mehta, A. Birerdinc. A. Baranova
Adipose tissue has been implicated in the complex metabolic relationship giving rise to metabolic syndrome. Adipokines seem to be involved in numerous inflammatory pathways directly involved in the progression of numerous diseases, such as T2D, and NAFLD, under the general umbrella term of metabolic syndrome. Recent studies have suggested that PCOS maybe the ovarian manifestation of metabolic syndrome.
Our study aims to profile mRNA gene expression for obesity and inflammatory cytokine related genes in the adipose tissue of patients with or without PCOS. We expect to see differential gene expression of the targeted obesity and inflammatory cytokine related genes in patients with PCOS, particularly in the insulin signaling pathways.
RESULTS: in progress